Meet this 41-year-old patient who despite having Lipoedema, was lucky enough to be educated on the condition early in life by her mother, whose side of the family is prevalent with Lipoedema. The patient can even see photos as far back as her grandfather’s sister, who had a dainty upper body and enlarged legs, which sadly led her to become wheelchair bound.
The patient must also take into account her two young daughters as also being susceptible to developing the genetic condition.
For her personally, the patient was undergoing IVF which caused early menopause. She then saw a rapid and dramatic change in the size of her legs due to swelling, the patient describes the physical change in the two year period as “insane.”
At the request of her mother, the patient booked in with Dr Lekich for a formal diagnosis and was unsurprisingly confirmed to have Lipoedema. The knowledge did provide a sense of relief in that she had a greater understanding of her body, she knew why she couldn’t shift the weight in her legs or why she became so easily fatigued.
But she was equally overcome by a creeping anxiety of what she was walking into. The patient recalls, “I knew that it was going to be a rough journey, I knew it was going to be an expensive journey, which meant that a lot of our goals as a family had to be changed … so yeah it was a mixed feeling. Relief for sure, and then what was just going to lie ahead.”
The patient did have a great advantage however, as she was aware of Lipoedema for a long time she already implemented conservative management techniques, leading her to be in a great position to become surgically ready. Her dieting was particularly easy as she had minimal secondary obesity, Dr Lekich didn’t even have her undergo a ketogenic diet, quite atypical for most patients. Instead, the patient was more conscious of her food choices, and closer to the surgery dates she pursued a nutritionist familiar with Lipoedema to follow a more structured diet plan.
Conservative management issues the patient did encounter were with compression. She describes her relationship as “bittersweet,” as she acknowledges the necessity and benefits of compression, but the expense was quite a burden. She failed to fit into her flat knits at first, and had to use an alternative compression before reattempting the flat knits, which she did finally fit into.
“I actually now have the problem where I can’t sleep without them, I really get a bad night’s sleep when I’m not wearing them.”
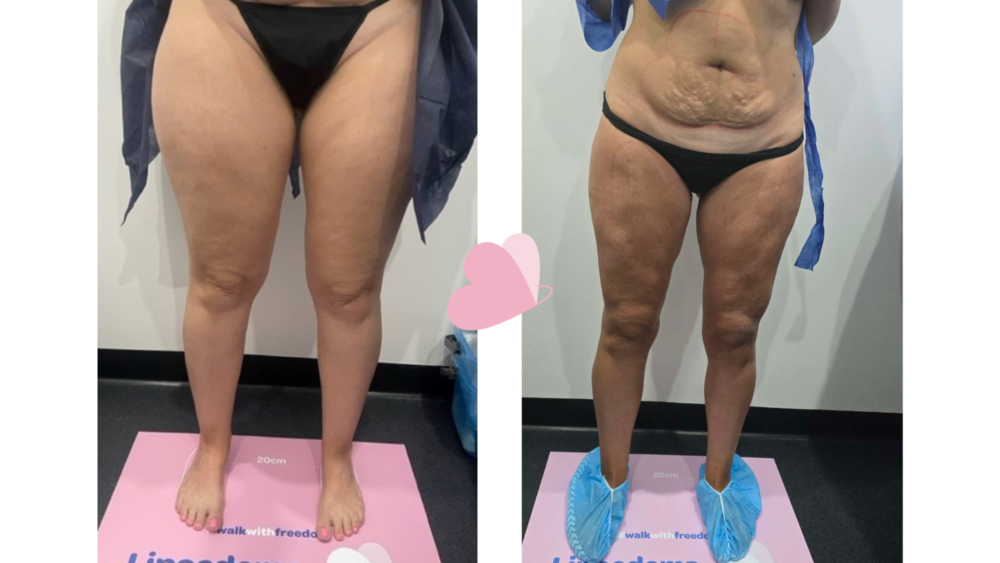
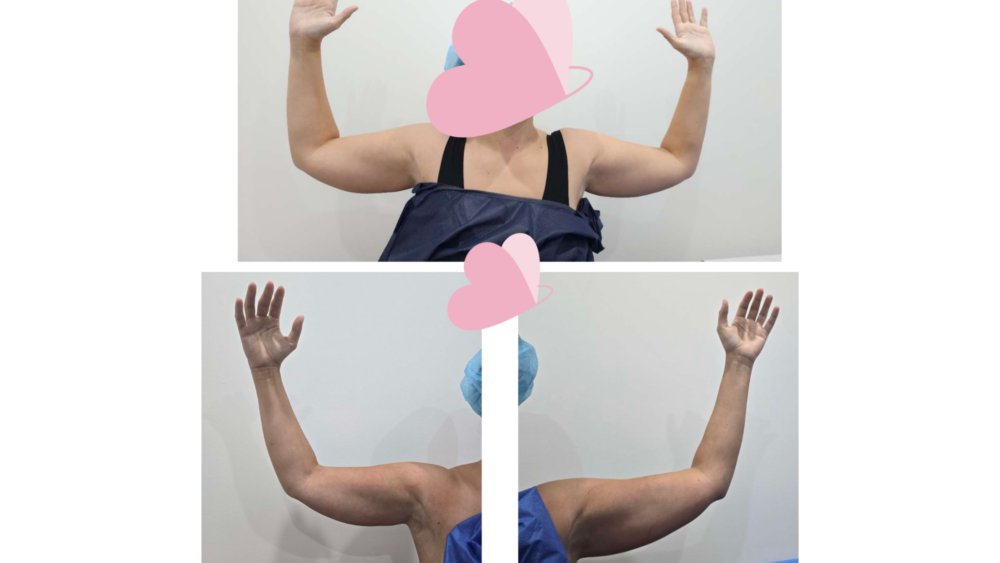
In August 2022, utilising a protocol to manage underlying venous disease and a Lymph-Sparing technique, a total of 2.4 litres of Lipoedema fat was removed from the patient’s lower legs by Dr Lekich. Subsequently in October 2022, a further 3.9 litres were removed from her anterior thighs and posterior thighs. The following year in April 2023, the patient had a further 1 litre removed from her arms and abdomen. Finally, she underwent a targeted Lipoedema revision and renuvion procedure to manage skin laxity / redundancy in February 2024, which saw 0.15 litres of fat removed.
Following the first two surgeries, the patient unfortunately didn’t receive the immediate mental and physical payoff she had dreamt of. It can take up to 12 months for results to manifest, and while she was aware of this, it was disheartening to have undergone physically, mentally, and financially stressful trials to see no results.
“It was just trusting the process, being very patient, and I only probably really started seeing results January this year … so it really took me five to six months of crying, training, crying, training, and not seeing results.”
In hindsight the patient noted room for improvement could be implemented in the post-operative care so that patients had realistic expectations of how their legs would appear during each time frame. Since her first procedures in 2022, patients now receive a comprehensive pre and post op guide with a roadmap for each step of the way.
Following this however, the patient is continually impressed by what her body can now do for her.
Previously her pilates instructor was dumbfounded by her lack of progress. When she should have been becoming progressively stronger, the opposite was occurring, getting to the point where she could barely lift her legs up. Post surgery however, the patient now has to remember to slow down as she can easily throw her legs up, and doesn’t need to use a quarter of the same force in her exercises as before.
The patient’s BMI was never a particular issue, and now she wants to focus on ways of becoming stronger. While she admits no one can ever be 100% happy when you have body dysmorphia, she can happily call her surgical journey finished and can benefit from the mental and physical outcomes which her ancestors were unfortunately never able to access.